30 Years of Periodontal Maintenance with Relapse and Cardiovascular Complications
By: Kendra Linders, RDH
January 31, 2019
The Challenge:
After decades of periodontal stability, the patient presented with a rapid advancement of pocketing and inflammation over a period of only 9 months.
The Background:
- Age: 60
- Sex: Male
- Medical History: Multiple medications for high blood pressure. Calcium channel blocker and angiotensin II receptor blocker and statin for cholesterol management. In 04/2018, patient had cardiac stents placed and was placed on a blood thinner.
- Family History: Immediate family history of cardiovascular disease. A sibling experienced heart attack.
- Last Dental Exam: 12/11/2018
- Home Care: Patient is highly motivated. Waterpik® daily with plaque seeker tip, Sonicare 2x/day
- Chief Complaint: “I feel like I’m starting to get a deep pocket around my implant.”
- Clinical Assessment: Gingiva was generally medium pink with rolled margins and spongy, erythematous papilla. Isolated severe inflammation visible at tissue around implant. Radiographs showed no pathology on implant and stable bone levels. Biofilm was minimal.
- Periodontal Assessment: Over a period of 9 months, the periodontal assessment showed an increase in 4-5mm pocketing from 4% to 18% with an isolated 9mm pocket on implant. Bleeding on probing increased from 2% to 10%. Using the 2017 AAP Periodontal Classification Guidelines, the patient was classified as having Stage III, Grade C generalized chronic periodontitis with isolated Stage IV due to pocketing at implant, rapid disease progression and cardiac risk.
Additional Comments: Patient was being seen on 4 month periodontal maintenance interval for past 10+ years. Scaling and root planing was first completed in 1980’s, with periodontal charting showing stable periodontium and indicating dormancy of disease over multiple decades. The patient’s cardiovascular inflammation was a likely contributor to the rapid shift in periodontitis activity.
The Solution:
- Date of Pre MyPerioPath (pre-therapy test): 9/13/2018
- Periodontal Therapy: 3 hour non-surgical periodontal therapy was performed including thorough scaling and root planing of all quadrants in a single visit. Post-scaling supra & subgingival polishing with glycine powder.
- Systemic Antibiotic Used: Systemic antibiotics were considered, however the one species above the Reference Line was low risk. We decided to move forward with treatment without supplemental antibiotic therapy. Patient was willing to consider antibiotics if pathogen(s) were persistent.
- Home Care: Daily Waterpik at level 8 for 2 minutes with extra time around implant. Sonicare 2x/day.
- Other Notes: Periosciences® AO Gel to use post-therapy with instructions to apply to all gingiva 3x/day until follow-up appointment.
- Date of MyPerioProgress® (post-therapy test): 12/11/2018
The Result:
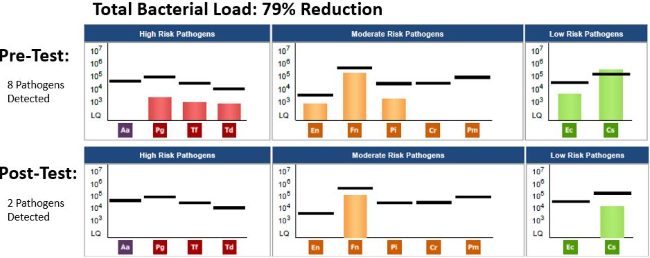
Clinical results showed a significant decrease in bleeding on probing and we were thrilled to see a reduction in implant pocketing from 9mm to 5mm and no bleeding. Generalized posterior pockets of 4-5mm were persistent at 18%. The MyPerioProgress report showed an overall bacterial load reduction of 79%. Careful monitoring with future MyPerioPath tests is indicated to ensure these pathogens remain at low levels.
This case exemplifies the need for frequent and close monitoring of all patients’ periodontal status. It also highlights the close link between systemic and oral inflammation. This patient’s periodontal condition had been predominantly stable for the past 30 years. As his cardiovascular health became more compromised, we saw a rapid shift in his oral stability, and an aggressive advancement of his periodontitis. Frequent periodontal assessments allowed us to identify and quickly treat this shift in periodontal disease activity. Moving forward, I hope to assess this patient’s host response and genetic inflammatory risk. While we know the patient has an increased risk of cardiovascular disease due to his family history, further genetic inflammatory marker testing with OralDNA®’s Celsus One™ would give us a more holistic picture of this patient’s true inflammatory risk.
About the Author:

As Director of Dental Hygiene, Kendra Linders, RDH works with patients individually to improve and maintain their oral health. Her goal is to support patients in achieving lifelong, whole-body wellness. She is passionate about education, and believes in developing a customized care plan that will work for each unique person.
Kendra brings 11 years of dental industry experience to the Seattle General Dentistry team. She holds an Associate of Science in Dental Hygiene from Shoreline College, and a Bachelor of Arts in Management Operations & Personnel Psychology from Washington State University. She is also a graduate of the Bale Doneen Preceptorship Course on the oral-systemic prevention of heart attack and stroke, and attends numerous continuing dental education courses each year.