Other
![Thumbnail [200x250]](img/case-study/Relapsed%20Periodontal%20Maintenance%20Patient%20with%20Breast%20Cancer%20Image_98406038%20%281%29.jpeg)
Relapsed Periodontal Maintenance Patient with Breast Cancer
The Challenge:
A periodontal maintenance patient of record presented past due for re-care. The initial exam revealed signs of active periodontal disease indicating that the patient is no longer in periodontal remission. Medically, the patient is undergoing treatment for breast cancer.
The Background:
- Age: 54
- Sex: Female
- Medical History: Hysterectomy; Breast cancer diagnosed Spring 2019, Cancer treatment included surgery and chemotherapy; cold sores; heart murmur; psychiatric care; ex-smoker
- Last Dental Exam: 6/05/2019
- Home Care: Fair/poor
- Chief Complaint: "I have slipped with my home care since all of this medical stuff happened."
- Periodontal Assessment: 1-5mm generalized pink and brown pigmented (due to ethnicity) attached gingiva; rolled gingival margins; blunted papilla
- Medical Assessment: Patient presents as ASA 2; active, mobile, trying to improve health since cancer diagnosis
The Solution:
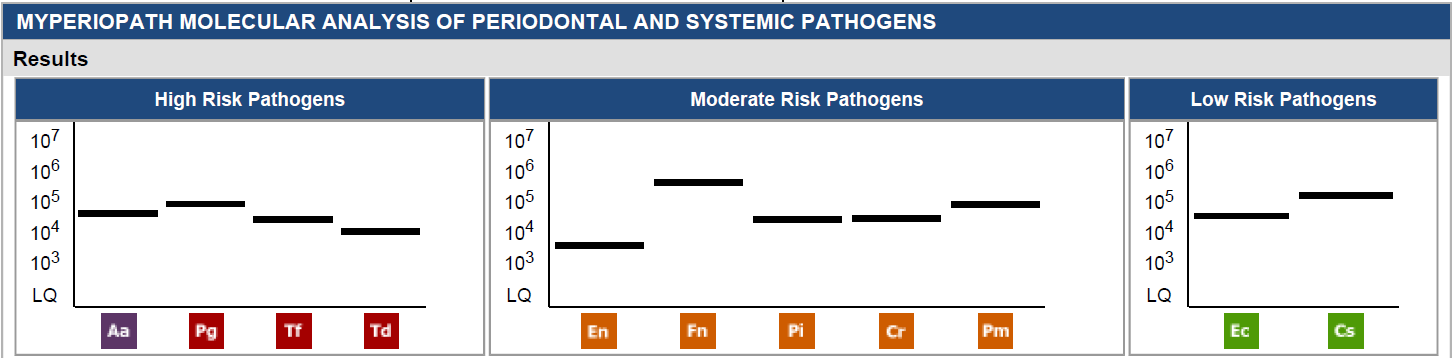
- Date of Pre MyPerioPath® (pre-therapy test): 8/19/2019
- Periodontal Therapy: Localized scaling and root planing to 5mm, Atridox® application to reduce inflammation
- Systemic Antibiotic Use: Not used due to insignificant levels of bacteria
- Home Care Instruction: Instructed to use Waterpik®
The Result:
I submitted this case study before the patient returned for the re-care appointment because I wanted to highlight how the MyPerioPath results streamlined my therapy. Originally looking only at the clinical signs of disease, I would have assumed there was a significant bacterial cause and both myself and the patient were prepared to include systemic antibiotics in the therapy. However, when the MyPerioPath results showed minimal bacteria, I then understood most of the inflammation was due to what the patient was experiencing in her overall health. I was able to provide personalized therapy for this patient.
About the Author:

Maria is a 2013 graduate of dental hygiene from Community College of Baltimore County, Dundalk. She is a licensed registered dental hygienist in the state of Maryland and currently working for a private practice in Annapolis. In her free time, she enjoys rock climbing and riding dirt bikes with her fiancé Chris.
![Thumbnail [200x250]](img/case-study/Traditional%20Periodontal%20Disease%20Case%20Study%20Blog%20Image_274116188%20%281%29.jpeg)
Traditional Periodontal Disease Case Study
The Challenge:
Patient with extremely limited history of dental care presents seeking dental wellness. Although patient is anxious, she is highly motivated to create a healthier dental foundation.
The Background:
- Age: 33
- Sex: Female
- Medical History: Seasonal allergies and anemia
- Last Dental Exam: 1/01/2019
- Home Care: Manual tooth brushing 1-2 times per day, occasional flossing
- Chief Complaint: Patient is motivated to achieve better dental health
- Periodontal Assessment: AAP Case Type II with localized 1-2 mm of recession, bleeding on probing was moderate with localized heavy bleeding sites
- Medical Assessment: BP: 111/71 pulse: 69
Additional Comments: The patient has limited recollection of any dental care in her life, even in childhood.
The Solution:
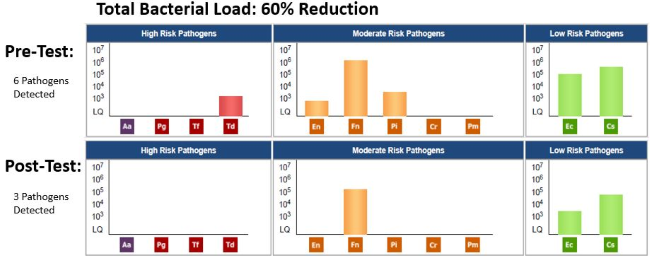
- Date of Pre MyPerioPath® (pre-therapy test): 1/08/2019
- Periodontal Therapy: Two visits consisting of scaling & root planing with ultrasonics, diamond files and laser assisted therapy
- Systemic Antibiotic Use: Considered, never administered
- Home Care Instruction: Instructions were given at every visit. The patient showed great improvement at every visit
- Date of MyPerioProgress® (post-therapy test): 4/04/2019
The Result:
It was rewarding the see the patient come in for the second half of her gingival therapy, as she was very motivated to maintain her overall oral health. She continues to be diligent in her efforts to make it to her dental visits. Scaling with the ultrasonic system went very well and the patient did not experience any sensitivity in the areas of recession. This patient’s case study was very rewarding. These pre- and post-treatment lab reports allowed me to better assess and evaluate the treatment we provided during the patient’s gum therapy in January 2019.
During the patient’s definitive therapy visit in April, it was rewarding to see that the patient had gained some clinical attachment with a decrease in her probing depths of 5 mm to 4 mm as well as a decrease in areas of bleeding on probing. She is very motivated and has made a strong attempt to implement routine oral care.
About the Author:

Dr. Brian Davey comes from a family of dentistry. His uncle, who was also his mentor, was a pediatric dentist. He recognized early on that Dr. Davey had the skill, both technical and interpersonal, to become a good dentist.
He earned his undergraduate degree from the University of California, Irvine, then attended the University of California San Francisco School of Dentistry from 1996-2000.
Dr. Davey has been designated as a Fellow for the Academy of Oral Systemic Health. He was also recognized as a Top 10 General Dentist in San Diego’s Best Union-Tribune Readers Poll (2019). Previously, he was awarded the 2014 Doctor of the Year for Next Level Practice Complete Health Dentistry, also earning a leadership award.
Today, Dr. Davey’s mission is to enhance people’s lives through health, wellness, and fun. He is committed to making a difference in the health of the San Diego community by getting 20,000 people healthier before 2020.
He believes the mouth is connected to the body, the body is connected to the family, and the family is connected to the health of a community. With that knowledge, his mission is bringing together the medical and dental community to collaborate for the greater good of San Diego and his patients.
In addition, he is the founder and creator of the San Diego Academy of Systemic Health (SDASH). In 2018, he won an award as a leader of complete health for creating SDASH and for working toward his 2020 goal of making San Diego America’s healthiest city.
Dr. Davey says, “I invite you to join my practice and become part of our patient family. I look forward to providing you with beautiful, healthy smiles now and for years to come.”
![Thumbnail [200x250]](img/case-study/sneed_wilson_03272019/Periodontal%20Therapy%20Without%20Pharmaceuticals%20Image-2.jpeg)
Periodontal Therapy Without Pharmaceuticals
The Challenge:
A patient of record with a history of prostate cancer is exhibiting active signs of periodontal disease.
The Background:
- Age: 69
- Sex: Male
- Medical History: History of prostate cancer, atrial fibrillation and cardiac ablation
- Last Dental Exam: 10/24/2017
- Chief Complaint: "I want to be proactive and per my functional medicine doctor, there could be bacteria complicating my overall health."
- Periodontal Assessment: 5-6 mm probe readings
The Solution:
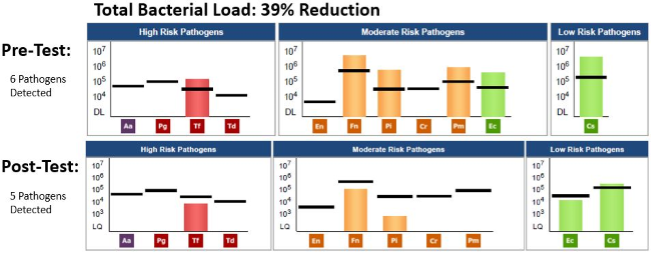
- Date of Pre MyPerioPath® (pre-therapy test): 6/20/2018
- Periodontal Therapy: Quadrant scaling and root planing augmented with laser and ozone; all performed 1 week apart.
- Home Care Instruction: Hydro Floss® oral irrigator, TePe® interproximal brushes to apply ozone oil at bedtime, Tooth & Gum® toothpaste and Jarrow Formulas® probiotics
- Perform MyPerioProgress® (post-therapy test): 2/04/2019
The Result:
Once therapy was applied and the patient healed for 12 weeks, the MyPerioProgress results revealed a 39% reduction in periodontal pathogens. Please note the reduction was obtained naturally. No systemic pharmaceuticals were ever used. Clinically, the patient has no bleeding on probing and all pockets are 3 mm or less. He continues to be diligent with his homecare utilizing the Hydro Floss and ozone oil. His PSA scores were still elevated in 2018; therefore, he continues to receive care in addition to a modified diet restricting all sugars (natural or refined) and all grains. We will continue to monitor him for active periodontal disease and continue to provide supportive therapy of full mouth ozone every 3 months. We will retest with MyPerioPath if the patient show signs of periodontal relapse.
About the Author:

Tonya Sneed is graduate of Howard College and has been practicing since 1987. At Dr. Tim Tannich's office she is the Total Body Wellness Coordinator, including the ozone department. Her passion as a career periodontal hygienist is showcased by her roles as a Soft Tissue Management consultant and a Health Coach. She has a background in Plantrician and attended Frontiers in Medical and Dental Ozone.
Michelle Wilson is a graduate of UT Houston and has been practicing since 1991 and is the clinical periodontal hygienist for Dr. Tim Tannich.
Both hygienists have advanced laser training from WCLI, have Advanced Ozone Training, and consult with other dental offices in the implementation of Ozone and LAPT. Both have attended Perio Passion and AAOSH.
![Thumbnail [200x250]](img/case-study/Gingival%20Hyerplasia%20with%20Bone%20Loss%20and%20Anor...%20Image_159509625.jpg)
Gingival Hyperplasia with Bone Loss and Anorexia Nervosa
The Challenge:
A 15-year-old patient with multiple years of periodontal concerns being co-managed with a periodontist without resolution.
The Background:
- Age: 15
- Sex: F
- Medical History: Behavioral concerns, at age 15 has not begun menstruation
- Home Care: Chronic poor home care
- Periodontal Assessment: History of referral to periodontist before orthodontics with minimal resolution. After orthodontics were removed, the radiographs revealed more bone loss. Referral to periodontist again. When patient appointed for maintenance care revealed gingival hyperplasia along with pliable gingival margins.
Additional Comments: Her appearance was pale and very thin. The mother reports for several years being unable to motivate the patient in areas of oral and personal hygiene.
The Solution:
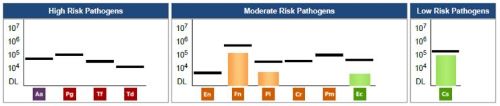
- Date of Pre MyPerioPath® (pre-therapy test): 6/20/2018
- Periodontal Therapy: Recommended 4 quadrants of scaling and root planing
- Other notes: Possible low dose doxycycline if inflammation persists
- Recommended to perform MyPerioProgress® (post-therapy test)
Additional comments: This treatment plan/solution was proposed but never completed.
The Result:
Therapy has been suspended. In consult with the mother about the MyPerioPath results and the recommended treatment plan, the mother reluctantly revealed the daughter was diagnosed with anorexia nervosa. I informed the mother I would be forwarding the test results to the daughter's pediatrician and periodontist. She made me aware that the daughter's Vitamin D level was very low and being tested every other day. In addition the daughter’s thyroid and hormone levels were significantly low too. The mother stated the daughter is now in a 6-week eating disorder program followed by outpatient care. The mother agreed to therapy once the eating disorder is under control. Upon a visit by the mother for another sibling’s care, the mother stated the daughter was improving but still has a long way to go.
I am appreciative of the level of care and concrete information I can now provide to my patients by utilizing OralDNA® salivary testing services. In conclusion, the underlying cause for this patient’s gingival hyperplasia and low to moderate bone loss is anorexia nervosa. Early in this patient’s care, I was suspicious there may be some depression concerns. This in addition to the clinical signs was a reason for referral to the specialist and a non-conclusive diagnosis. Now with testing I can rule in or rule out bacteria being a cause for the inflammation so we can explore other possible reasons for the inflammation and provide more timely care.
About the Author:
