Periodontitis
![Thumbnail [200x250]](img/case-study/Class%20II%20Periodontitis%20and%20Mouth%20Breathing_124787499_v2.jpg)
Class II Periodontitis and Mouth Breathing
The Challenge:
To establish health through periodontal intervention per JP Institute protocols.
The Background:
- Age: 25
- Sex: Female
- Medical History: Adderall controlled ADHD with panic disorder
- Family History: Father: early Cardiovascular Disease; Maternal Grandmother: periodontal disease and high decay rate; Maternal Grandfather: died in his 60's of fatal myocardial infarction, history of transient ischemic attack, oral cancer and lung cancer
- Last Dental Exam: 3/02/2016
- Chief Complaint: Gums hurt and bleed, bad breath, mouth breathing
- Clinical Assessment: Referral to periodontist 3/2/2016. Diagnosed with Localized Aggressive Periodontitis. Recommended Treatment: Surgery with fair prognosis. Patient scheduled for surgery but canceled the appointment. Recommended third molars extracted, but never scheduled.
- Periodontal Assessment: Generalized 4-5mm pockets with bleeding, localized 6-9mm pockets, radiographic bone loss.
The Solution:
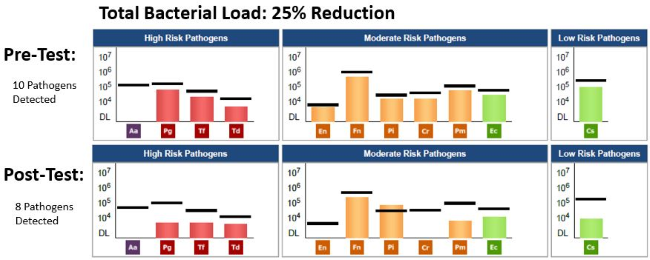
- Date of Pre MyPerioPath® (pre-therapy test): 4/20/2017
- Periodontal Therapy: 6-8 one hour Periodontal Therapy Visits, Micro-ultrasonic technology, Oral Irrigation, Extraction of partially erupted 3rd molars.
- Systemic Antibiotic Use: Metronidazole 500mg bid for 8-10 days
- Home Care Instruction: Sonicare Toothbrush & Sonicare Airflosser, StellaLife® rinse and gel, LifePak® Nano
- Date of MyPerioProgress® (post-therapy test): 8/30/2017
Additional Comments: The post therapy test was ordered as an Alert 2™. Nutritional Counseling was also administered.
The Result:
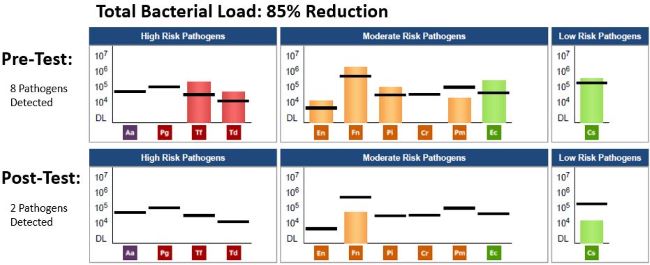
By incorporating OralDNA salivary tests, the pre-test MyPerioPath, and integrating The JP Institute methods of communication, my patient was able to own her disease. The pre MyPerioPath confirms a bacterial cause and the post MyPerioProgress gives an objective measurement of bacteria reduction. The MyPerioID® portion of the Alert 2 being G/G, or High risk, helps to establish the need for more comprehensive non-surgical therapy and frequent re-care as well as forewarns the patient of possible relapse.
I was confident the periodontal therapy was going to result in a healthy tissue response, which is apparent from the below photo. The patient and I were pleasantly surprised with the overall health benefits including improved energy, better breathing- as her sinuses cleared resulting in secession of mouth breathing, and her mood stabilized resulting in discontinuation of Adderall.

About the Author:

Annie-Laurie Harris BSDH, RDHMP has been in clinical practice for 22 years. Her career began in a progressive periodontal specialty practice where she developed a fascination for the treatment and maintenance of periodontal disease. She was introduced to a philosophy and technique that was innovative and successful in treating periodontal disease. She received intensive training from the JP Institute in Evolutionary Hygiene in 2004. In 2008 she completed JP Institute's Mastership program. She is also currently pursuing a Master's Degree in Dental Hygiene Research at Old Dominion University.
She became a founding member of the American Academy of Oral Systemic Health. This discovery ignited an enthusiasm for the science and treatment of biofilm. Her colleagues and patients have given her the affectionate nick-name 'Dental Geek'. She has been known to attach a head cam to demonstrate (to her willing patients) live video of the biofilm disruption process. Annie is thrilled to be mentoring and training to her fellow colleagues and considers herself a JP Institute Evangelist.
![Thumbnail [200x250]](img/case-study/Class%20II%20Generalized%20Periodontitis%20and%20Rheumatoid%20Arthritis%20Requesting%20Implant%20Placement_328261126-RESIZE.jpeg)
Class II Generalized Periodontitis and Rheumatoid Arthritis Requesting Implant Placement
The Challenge:
To establish periodontal remission by addressing the clinical manifestations of periodontal disease and altering the oral flora in order to lower the incidence of periodontal disease relapse. Bacterial management will eliminate a source of total body inflammation and increase success of implant placement.
The Background:
- Age: 66
- Sex: Male
- Medical History: Rheumatoid arthritis, takes Lisinopril
- Last Dental Exam: 05/16/2019
- Home Care: Brushing twice a day and sporadic flossing
- Chief Complaint: Missing tooth #19 and interested in dental implant
- Clinical Assessment: Class II generalized periodontitis with localized Class III periodontitis. Generalized bleeding on probing and localized bulbous and erythematous tissue on buccal aspect of tooth #5 due to excess material on Class V restoration.
- Periodontal Assessment: Upon probing and completion of periodontal assessment, this case was classified as Class II generalized periodontitis with localized Class III periodontitis due to pocket measurement on mesial of #14.
Additional Comments: Patient indicates he visits the dentist every six months and reports no previous periodontal treatment.
The Solution:
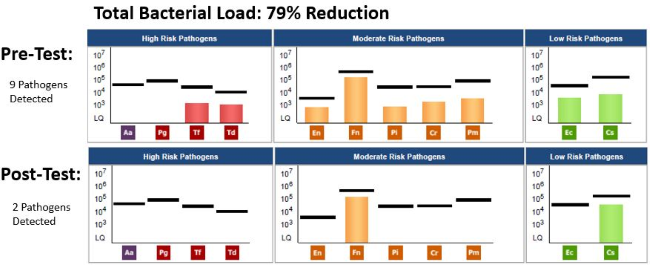
- Date of Pre MyPerioPath® (pre-therapy test): 05/16/2019
- Periodontal Therapy: Patient was scheduled for full mouth debridement and localized curettage on periodontal pocket sites. This procedure was performed for 3 consecutive weeks and pockets were stabilized to measurements 2-3mm.
- Systemic Antibiotic Use: A script of Amoxicillin 500mg, 3 times a day for 7 days was prescribed even though all bacteria were under reference lines.
- Home Care Instruction: Perio Protect™ trays were recommended for use twice a day with Perio Gel® for 15 minutes each application for 3 weeks, then every other day until 3 month follow-up. Oral hygiene instructions on how to brush and floss correctly were reinforced.
- Date of MyPerioProgress® (post-therapy test): 09/03/2019
The Result:
Clinically there was 100% pocket size reduction on pockets greater than 3mm. All periodontal pockets stabilized and zero bleeding on probing was observed. There was a 79% reduction in periodontal pathogen (burden) load 3 months and 18 days after treatment started. These current results are likely associated with a decrease in both oral and systemic inflammation. Having clinical improvement is always our goal and was achieved in this case. The significance of having the pre and post therapy MyPerioPath results gives me an objective measurement to things I can’t visually see. With the reduction of bacterial load, I now know the environment for surgical placement of an implant has less risk for failure due to periodontal pathogens. I utilize this test as a pre-surgical work up, just like a medical doctor uses blood work before their hip/knee/valve replacements surgeries.
About the Author:

Dr. Patricia Lugo is a Puertorriquena oral surgeon who studied her doctorate degree at University of Puerto Rico Medical Sciences Campus and has been practicing for more than 10 years in the private sector. Her passion is practicing Complete Health Dentistry, dentistry that links oral health with systemic health. She works with her husband, Dr. Edwin Rodriguez, prosthodontist, on providing optimal health to patients with complex oral rehabilitations.
![Thumbnail [200x250]](img/case-study/Class%20III%20Moderate%20Periodontitis%20with%20Halitosis%20Case%20Study%2030%20Percent%20Fade_68322631.jpg)
Class III Moderate Periodontitis with Halitosis
The Challenge:
To reduce periodontal pathogens, a significant cause for the periodontal inflammation and halitosis.
The Background:
- Age: 61
- Sex: M
- Last Dental Exam: 3 months ago
- Home Care: Manual toothbrush daily and flossing on & off
- Chief Complaint: Halitosis
- Periodontal Assessment: Type III generalized with localized Type IV periodontitis. Patient has history of periodontal therapy in past with 3 month re-care intervals. The patient had generalized heavy, bleeding on probing and tissue was bulbous & erythematous.
The Solution:
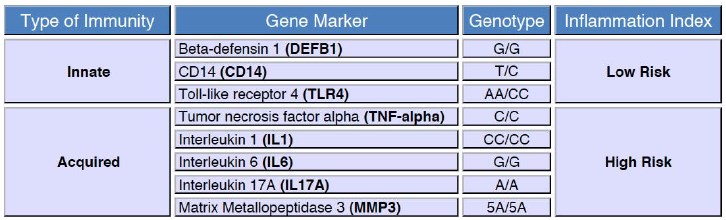
- Date of Pre MyPerioPath®, Celsus One™ and OraRisk® HPV on 7/13/2017
- Periodontal Therapy: Initially recommended 12 hrs of non-surgical periodontal therapy due to Celsus One High Inflammation Index. However, only 4 hrs were needed due to patient’s home care compliance (see Home Care below). The therapy consisted of microsonics, irrigation and laser therapy.
- Systemic Antibiotic Used: It was considered but due to the patient's favorable response to non-surgical, it was never administered.
- Home Care: PerioProtect™ trays 2-3x/day with a vibramycin (doxycycline gel) for 6 weeks initially. Following the non-surgical periodontal therapy, PerioProtect trays 2x/day with 1.7% peroxide gel, Waterpik® daily and electric toothbrush 2x/day.
- Date of MyPerioProgress® (post-therapy test): 11/09/2017
The Result:
Clinically there was a significant decrease in bleeding on probing and pocket depth reduction was amazing. The MyPerioProgress showed pathogen reduction from 8 above reference line to 0. I enjoy seeing the patient’s reaction when they realize they have some control over what is happening. When they do the expected increased home care and reduce therapy time, they are thrilled. This re-enforces home care for maintenance. In this case, the patient’s partner was tested and revealed periodontal pathogens very similar to this patient, however the partner has refused treatment at this time. This places our patient at risk for relapse especially due to the Celsus One results.

About the Author:

![Thumbnail [200x250]](img/case-study/LIGHT%20Class%20II%20Periodontitis_130547494.jpg)
Class II Periodontitis
The Challenge:
The patient has Class II periodontitis with a lack of home care and recall. Through periodontal therapy, our goal is to establish a remission of the disease and establish a healthier bacterial load to reduce oral/systemic complications. Through education, our goal is to establish home care habits to assist patient’s remission and stress the need for recall not just for health of periodontium but overall health.
The Background:
- Age: 54
- Sex: F
- Medical History: High blood pressure and allergy to penicillin
- Family Medical History: Diabetes, cardiovascular disease, stroke and cancer
- Last Dental Visit: 6 years ago
- Home Care: Manual toothbrush 1-2x per day with occasional antibacterial mouth rinse and tongue brushing
- Nutrition: Diet soda daily, tea with honey
- Patient Chief Complaint: “Bleeding gums when brushing, possible cavities and tooth crowding.”
- Clinical Assessment: Deteriorating margins of amalgam restoration, recurrent decay diagnosed by exam and radiographs. Generalized plaque with moderate calculus.
- Periodontal Assessment: Class II periodontitis. 110 out of 168 points of bleeding, all 28 teeth with generalize 4 mm probe depths with localized 5mm probe depths. Bone loss of 1-10% including both horizontal and vertical throughout.
The Solution:
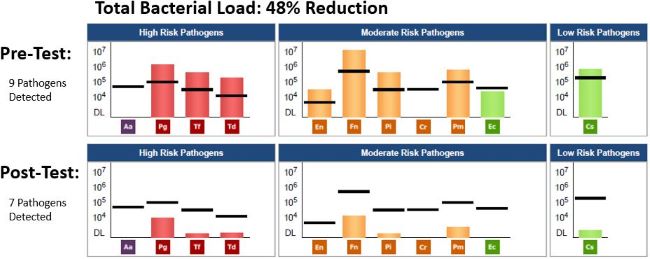
- Date of Pre MyPerioPath® (pre-therapy test): 6/15/2017
- Periodontal Therapy: 4 quadrants scaling and root planning and doxcycline subgingivally in all areas.
- Systemic Antibiotics Used: Ciprofloxacin & Metronidazole per results
- Home Care: Chlorhexidine rinse at home 2x daily
- Date of MyPerioProgress® (post-therapy test): 10/5/2017

The Result:
At the 6-week tissue check, this patient has been using an electric toothbrush 1-2x per day, flossing a couple times per week, utilizing a tongue scraper, and using the chlorhexidine mouth rinse. Patient discontinued the rinse after 2 weeks due to increasing sensitivity. Post-therapy periodontal charting was completed with 1 localized 4mm residual pocketing and 12 out of 168 bleeding on probing. The post therapy MyPerioPath saliva sample was collected. A prophy, polishing, flossing was also completed. Patient will be seen every 3 months for periodontal maintenance. MyPerioProgress results showed reduced periodontal pathogens reductions from 7 pathogens above reference lines to 0 above. The patient was called, and results were reviewed, she then received a copy to give to her medical doctor.
About the Author:
