
Challenge: After decades of periodontal stability, the patient presented with a rapid advancement of pocketing and inflammation over a period of only 9 months.
Background: A 60-year-old male maintaining periodontal health for over 30 years started to relapse. Upon periodontal assessment, there were increasing pockets throughout, especially around an implant, of 9mm. The gingiva was generally medium pink with rolled margins and spongy, erythematous papilla with isolated severe inflammation visible at tissue around implant. Medically, there were significant updates too. The patient has a family history of cardiovascular disease with a sibling having a heart attack in 2018. This prompted the patient to investigate his cardiovascular risk. In addition to taking medication for high blood pressure and cholesterol, the patient had cardiac stents placed due to partial blockage and was put on a blood thinner. The patient’s cardiovascular inflammation was a likely contributor to the rapid shift in periodontitis activity. His chief complaint was “I feel like I’m starting to get a deep pocket around my implant.”
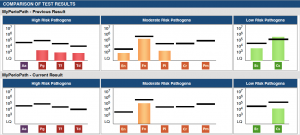
Solution: A pre-therapy, MyPerioPath® specimen was collected on 9/13/2018. Based upon the results a personalized treatment was developed to include 3 hours of non-surgical mechanical therapy including scaling and root planning and subgingival polishing with glycine powder. An extensive home care instruction including Waterpik®1x/day, Sonicare 2x/day and PerioSciences® AO Gel 3x/day was instructed. The systemic antibiotic option was considered but ultimately not administered. A MyPerioProgress® specimen was collected post-therapy on 12/11/2018.
Results: Upon reassessment, the clinical results showed a significant decrease in bleeding on probing and we were thrilled to see a reduction of the pocket around the implant from 9mm to 5mm with no bleeding. Still present is generalized posterior pockets of 4-5mm at 18%. The MyPerioProgress® report showed an overall bacterial load reduction of 79%. The bacteria remaining will be carefully monitored with future MyPerioPath® tests to address these pathogens, if and when they progress. Keeping all these bacteria at low levels is an objective of therapy in addition to reduced or zero inflammation.
This case exemplifies the need for frequent and close monitoring of all patients’ periodontal status. It also highlights the close link between systemic and oral inflammation. This patient’s periodontal condition had been predominantly stable for the past 30 years. As his cardiovascular health became more compromised, we saw a rapid shift in his oral stability, and an aggressive advancement of his periodontitis. Frequent periodontal assessments allowed us to identify and quickly treat this shift in periodontal disease activity. Moving forward, I hope to assess this patient’s host response and genetic inflammatory risk. While we know the patient has an increased risk of cardiovascular disease due to his family history, further genetic inflammatory marker testing with OralDNA®’s Celsus One™ would give us a more holistic picture of this patient’s true inflammatory risk.
For more information on how to become an OralDNA Provider – scan HERE: 
