 “How Do You Speak Testing” provides insight into how to talk with your patients about optimal care. The guest author has been given a fictitious patient with background information and clinical signs along with a randomly selected test result(s). The guest author will share their expertise in communicating OralDNA® Labs testing with patients.
“How Do You Speak Testing” provides insight into how to talk with your patients about optimal care. The guest author has been given a fictitious patient with background information and clinical signs along with a randomly selected test result(s). The guest author will share their expertise in communicating OralDNA® Labs testing with patients.
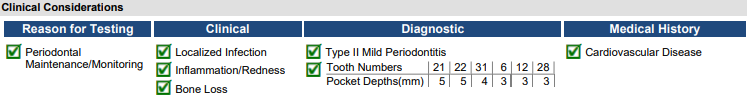
Hypothetical Patient Bio: An 82-year-old female patient has been seeing you for periodontal maintenance. She has cardiovascular disease, takes lisinopril and a prescription blood thinner. She is a smoker. Upon your clinical exam: inflammation, redness, bone loss, and generalized 3 to 5 mm pockets around the lower left premolar area were discovered.
Introduce testing to the above hypothetical patient.
Becky Comstedt RDH: Good morning Ms. Smith. After reviewing your oral health today, I’m seeing some unresolved inflammation around your lower left teeth. I know that we’ve been seeing you frequently to maintain your oral health and we’ve tried to incorporate a variety of tools that are easy for you to use at home, but this inflammation is a sign that we may need to utilize a different approach.
I know that you take a blood thinner, and your gums may bleed more easily, but the inflammation localized on your lower left may be a sign of a bacterial infection that we need to address. I recommend that we test your saliva to make sure this isn’t an indication of a more serious bacterial infection. [Here I would use a visual aid showing the bacteria often found in periodontal disease/gingivitis with the systemic signs and symptoms]
Once we have the results back, I will review them with you and together we can decide the best course of action.
MyPerioPath® Test Results:
Interpret MyPerioPath® results for the hypothetical patient.
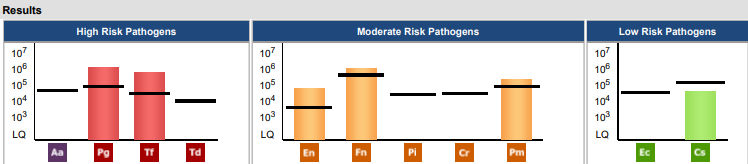
Becky Comstedt RDH: Ms. Smith, I am so glad you chose to test your saliva! We would have been “spinning our wheels” had we not identified the specific bacteria in your mouth. The first thing I noticed when I saw your results is that you do have high risk bacteria that are unfazed by the treatment we’ve been performing thus far. Interestingly enough, both bacteria are associated with heart disease. It’s likely that a source of your cardiovascular disease is right here in your mouth! While we cannot undo the damage that’s been done, wouldn’t it be great to minimize future damage?
The other finding these results reveal, is that your mouth is colonized with many of the moderate risk pathogens that are more common in smokers.1 I understand smoking is a difficult habit to break, and I’ll offer some solutions that you can hopefully easily embrace. If you would like to consider quitting smoking, I’d love to talk more about that!
So, let’s talk about options moving forward. While I’m not generally an “antibiotics first” type of practitioner, I do think that in your case, with the high levels of these dangerous bacteria, it’s best to utilize antibiotics. Fortunately, based on your MyPerioPath® lab report we can prescribe ones specific to these bacteria! How do you feel about that?
Additionally, vitamin E (a-tocopherol) may have benefits against one of the bacteria in your mouth (Pg).2 I’d suggest you talk to your MD about the right vitamin E dosage for you, as it is one of the vitamins that can accumulate in your body if you take too much. When are you due for your next primary care physician appointment? Would you like me to write something for them, or are you okay bringing it up?
When you come for your recare appointments, I’d like to start using the laser each time. We’ll try to reduce the bacteria numbers at their source, which is under the gums. In 6 months, we need to retest to verify that we are on the right track! How do you feel about this plan, Ms. Smith?
References:
For more information on how to become an OralDNA Provider – scan HERE: 
This is a hypothetical case and should be used for educational purposes only.
- How Do you Speak Testing? With Becky Comstedt RDH - July 30, 2021