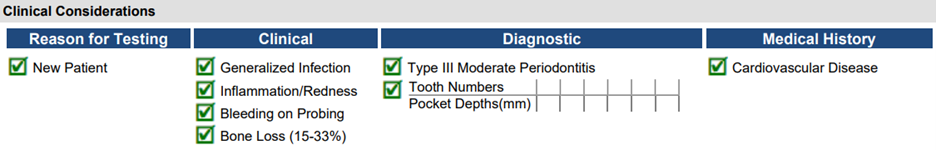
Patient Bio: A new patient, female, age 41 appointed to your practice. Upon medical history review, she is currently not taking any medications, only nutritional supplements recommended by her dietician. Her family history revealed her father has cardiovascular disease and sister has Type 2 diabetes. Completing the periodontal assessment identified:
How would you introduce therapy including MyPerioPath® to this patient?
(Patient) we understand that the health of our mouths and the health of our bodies impact one another in many ways. What we know is that there are numerous bacteria in our mouths that are linked to gum disease and other systemic diseases. Unfortunately, what we know now is that not just one form of treatment is enough to eliminate or reduce oral pathogen levels.
We believe in being as thorough as possible and customizing your care to help you obtain and maintain optimal oral health. So, why don’t we consider salivary testing to delve into this deeper? This will test for bacteria that can be closely linked to cardiovascular disease and diabetes. I have concerns about the symptoms I’m seeing and cardiovascular disease and diabetes being in your family history.
How would you discuss these results with your patient, your treatment plan and the need to retest?
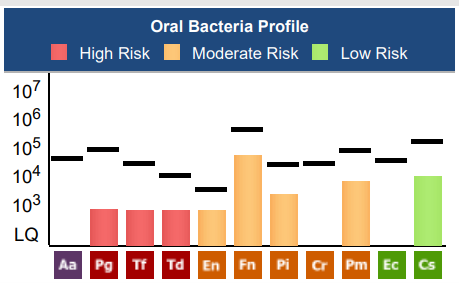
Among the 11 different pathogens we tested for, 8 were found in quantities exceeding 500. The other three pathogens may not be completely absent, but they did not surpass the testing threshold.
When it comes to systemic effects and the oral cavity, you have 5 out of the 6 bacteria that relate to heart disease. Your heart is just 12 inches from your mouth. The vessels in your gums lead to the heart, making it an easy way for cholesterol and other lipids to deposit. This can lead to inflammation in the arteries the same way our gums become inflamed. The inflammation in our arteries can lead to a heart attack, and with your family’s history, I would really advise taking every precaution in treating these bacteria that are closely related.
Now relating to your family’s history of diabetes, you present with 4 out of the 5 bacteria that are closely related to damaging the pancreas where insulin is produced. Inflammation is another big factor here and that’s what damages the pancreas. Unfortunately, with diabetes, slow wound healing is a symptom, and this greatly affects the mouth. Luckily, diabetes has not been diagnosed yet – so let’s talk about how to treat your oral infection in order to help reduce the risk of developing diabetes.
Based on what I’ve observed, the best form of treatment to start with is a deep cleaning. This will help us disrupt as much bacteria as possible and remove any irritants, such as tartar, below and above the gum line. During that visit, I also suggest a gentle gum irrigation with an antimicrobial solution, which many patients find soothing. For the bacteria that are tissue invasive and not effectively addressed by a deep cleaning (Pg, Tf, Pm, Pi), laser decontamination is an ideal approach.
After this treatment, I recommend at home ionizing perio trays to continuously combat these bacteria. It’s important to remember that our in-office procedures are just one part of the solution. The question is, how will you manage these pathogens at home to keep them in remission? That’s where these perio trays come in. I’d also like you to use probiotics that are designed for the oral cavity throughout the day.
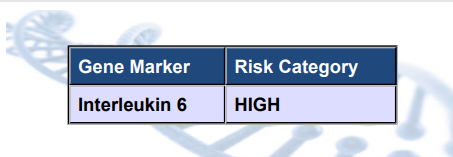
Now, in regard to your IL-6 being high risk, I’d advise you to consult with your primary care doctor on your vitamin D levels. Given the ‘high risk’ results, I’d like to see vitamin D levels within a range that many doctors typically wouldn’t look for. Considering your lab results, I find this step imperative.
Lastly, once this treatment has been completed, it is crucial to check the effectiveness of the treatment. The best way to determine this is to retest these bacteria levels 6-12 weeks after your treatment.
- How Do You Speak Testing? With Karina Diaz, BASDH, CRDH - August 25, 2023