Challenge: To establish periodontal remission by addressing the clinical manifestations of periodontal disease and altering the oral flora in order to lower the incidence of periodontal disease relapse. Bacterial management will eliminate a source of total body inflammation and increase success of implant placement.
Background: The patient is a 66 year-old-male with rheumatoid arthritis, taking Lisinopril and is a potential candidate for implant to restore #19. Patient’s daily home care routine includes brushing twice a day and sporadic flossing. Patient indicates he visits the dentist every six months and reports no previous periodontal treatment. Upon probing and completion of periodontal assessment, patient was classified as Class II generalized periodontitis with localized Class III periodontitis due to pocket measurement on mesial of #14. During probing there was generalized bleeding. Localized bulbous and erythematous tissue was observed on the buccal aspect of tooth #5, likely due to excess restorative material on Class V restoration.
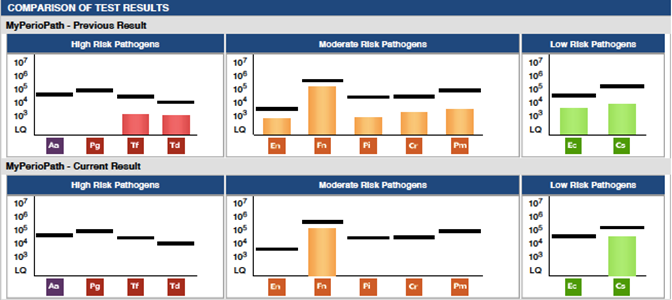
Solution: Our standard of care for patients presenting with generalized gingivitis to periodontitis is to perform a MyPerioPath® lab test. A saliva sample was collected on May 16, 2019 and submitted in order to identify the presence of periodontal disease-causing bacteria. Also, PerioProtect™ digital impressions were completed and sent for tray fabrication. The MyPerioPath® results revealed that the patient harbored 9 out of 11 periodontal disease-causing bacteria with a mixed flora of anaerobic and facultative microbes. By knowing which bacteria are present, we can address with specific antibiotics that will be most effective. Following the therapy (see next paragraph), a dosage of Amoxicillin 500mg, 3 times a day for 7 days was prescribed even though all bacteria were under levels of threshold. The goal is not only to treat gum inflammation but to also change the oral flora. Dentists can treat periodontal pockets and bleeding but if the aggravating agent is still present in the mouth there is a higher probability of disease relapse.
PerioProtect™ trays were recommended for use twice a day with perio gel (hydrogen peroxide gel) for 15 minutes each application. Oral hygiene instructions on how to brush and floss correctly were reinforced. The actual periodontal therapy occurred over 3 consecutive weeks and consisted of full mouth debridement and localized curettage on periodontal pocket sites and the above systemic antibiotic. New maintenance instructions were given to use perio trays with perio gel every other day until the 3 months follow up appointment. A post-therapy MyPerioPath® saliva sample was collected on September 9, 2019, and a general cleaning provided.
Results: Clinically there was 100% pocket size reduction on pockets greater than 3mm. All periodontal pockets stabilized and zero bleeding on probing was observed. There was a 79% reduction in periodontal pathogen (burden) load 3 months and 18 days after treatment started. These current results are likely associated with a decrease in both oral and systemic inflammation. Having clinical improvement is always our goal and was achieved in this case. The significance of having the pre and post therapy MyPerioPath® results gives me an objective measurement to things I can’t visually see. With the reduction of bacterial load, I now know the environment for surgical placement of an implant has less risk for failure due to periodontal pathogens. I utilize this test as a pre-surgical work up, just like a medical doctor uses blood work before their hip/knee/valve replacement surgeries.
Would you like to view more case studies? Click here and choose a category.
We hope you enjoyed the throwback blog. This interview originally posted 12/06/2019.